
Summary
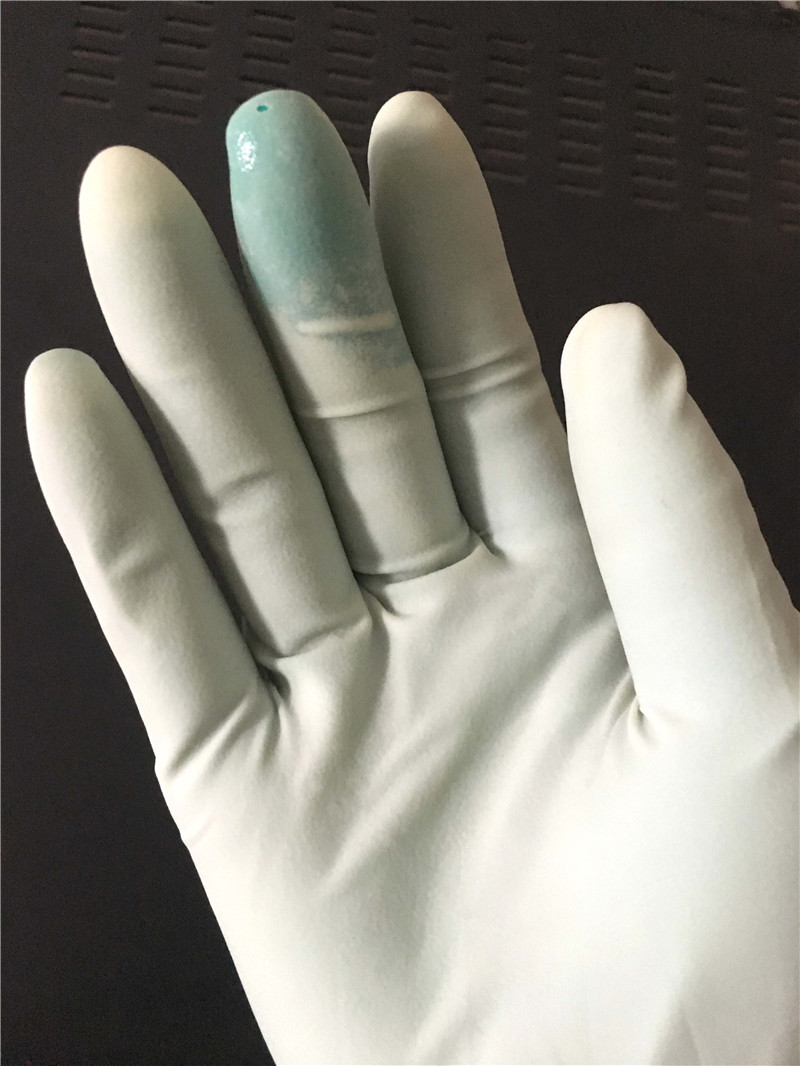
The stresses placed on a surgical glove today—the length of cases, heavy and/or sharp instrumentation, and chemicals used in the surgical field—make it imperative that barrier protection be ensured.
Background
The use of sterile surgical gloves has become the international standard of care in the perioperative environment. Yet the potential for barrier failure exists, with the subsequent potential for the transfer of pathogens to both the patient and the surgical team. The practice of double gloving (wearing two pairs of sterile surgical gloves) is often considered a mechanism for managing the potential risk of exposure during surgery.
Literature on double gloving
In the 2002 Cochrane review of double gloving, findings were summarized from 18 studies. The review, which covers a variety of surgical environments and addresses several double gloving options, indicates that double gloving significantly reduced perforations to the innermost glove. Other studies report a risk reduction of 70%–78% attributed to double gloving.
Overcoming practitioner objections
Practitioners, in voicing objections to double gloving, cite poor fit, loss of tactile sensitivity, and increased costs. An important issue is how the two gloves work together, especially when they are powder free. Several studies have reported good acceptance of double gloving without loss of tactile sensitivity, two-point discrimination, or loss of dexterity. Although double gloving increases the glove cost per practitioner, the reduction of bloodborne pathogen exposure and possible seroconversion of practitioners represents a significant savings. Strategies that may help to facilitate the process include sharing the data on double gloving to build justification for the implementation, enlisting the support of the champions of the change at hand, and providing a glove-fitting station.
Post time: Jan-20-2024